Acute Intermittent Porphyria (AIP)

 TO ALL THE ZEBRA CHASERS:
TO ALL THE ZEBRA CHASERS:
In medical training, many practitioners are taught the old saying, “When you hear hoof beats, think horses, not zebras”, which means that providers should consider the most likely possibility first when thinking of a dx.
I share the journey to raise awareness of this rare condition, improve compassion with providers to our patients, and decrease condition misdiagnosis. As a PA, one of the best parts of my training was thinking outside the box and going to other experts on what I needed help understanding; these happened when I self-advocated.
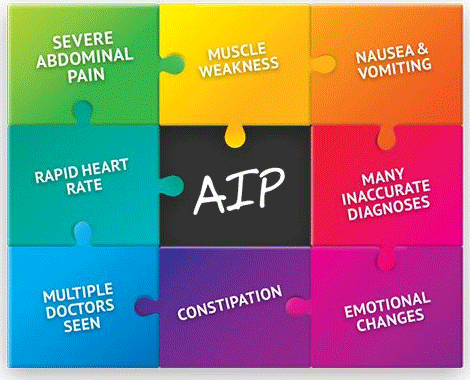
Over the past five years, I've been in many emergency rooms and inpatients with significant abdominal pain, neuropathy SIADH, ileus, and SBO. Multiple specialties along the way misdiagnosed me. They couldn't figure it out, and all were pretty frustrated; part of it, too, is that most severe concerns just vanished. The painful episodes varied, but all were intermittent; labs would return to normal and suddenly bizarre with hepatic and renal concerns that didn't seem reasonable considering the clinical vignettes.
Some providers thought it must be alcohol dependence, pain seeking, and malingering. I can't say that I haven't thrown some back with drinks but not in a range with dependence. Attacks didn't seem to happen with alcohol; many occurred without any apparent influences that may have clarified things. Many of the providers were hoping that this could be an easy box of a diagnosis and probably were burnt out with general conditions, unfortunately, and looked past the patient. In their defense, most people with this condition have emergent symptoms for 15 years before it is diagnosed. In these providers' neglect, patients with concerns they thought deserve better care.
February 2023, I began to suspect that the many physicians in my care were missing something, so I hit the books, PubMed out, and up-to-date maxed. I stumbled on a case study with an individual with a similar presentation with six hospitalizations and a few fewer organs in the abdominal cavity that had acute intermittent porphyria. Now for me, this is not a condition that I had heard of or on my radar, but I went through the differential and began to review labs that fit the clinical presentation of this condition. So I texted my close group and got my health provider to order some labs to see if we could catch this mystery as sometimes the labs out of attacks can clear, and boom figured it out with compelling labs. Even though I am a healthcare provider, many professionals have ignored my complaints for years. Having some satisfaction in figuring it out makes me feel a little better.
I may be the first PA that diagnosed themself with Acute Intermittent Porphyria. If anyone knows that other person, we need to connect for sure. Aside from that, the process has changed my perspective from hearing out each patient and not stop searching for what ever can help decrease suffering.